What is it?
Haemorrhoids are located in the submucosal layer in the lower rectum where they arise from a plexus of dilated arteriovenous channels and connective tissue which drain into the superior and inferior haemorrhoidal veins.
Haemorrhoids are thought be associated with straining and constipation with increased pressure causing engorgement and enlargement of the vascular system. Haemorrhoids may be common in men who have receptive anal sex.
External haemorrhoids occur below the dentate line.
Internal haemorrhoids occur above the dentate line.
Clinical presentation
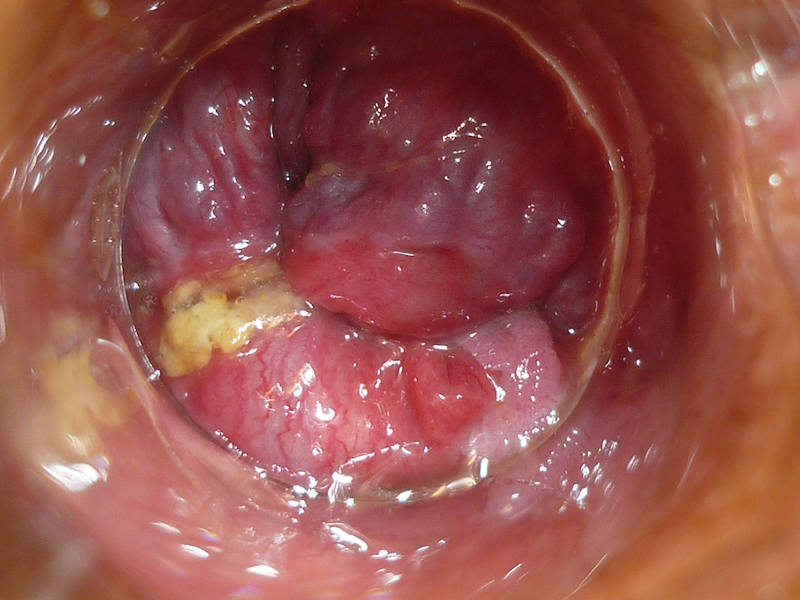
Haemorrhoids appear as soft, purplish masses which are seen with stretching the perianal skin or using the proctoscope.
The hallmark feature of haemorrhoids is painless bleeding noted on the toilet paper or in the toilet bowl.
External haemorrhoids
External haemorrhoids may thrombose and cause acute pain.
Healing external haemorrhoids may present as a firm, painless lump often associated with pruritus.
A skin tag commonly remains after an external haemorrhoid has resolved.
Internal haemorrhoids
Internal haemorrhoids form within the anal canal beneath the lining.
The most common symptoms are painless bleeding and protrusion during bowel movements.
Internal haemorrhoids are graded as:
- Grade I: visualised on anoscopy and may bulge into lumen but do not extend below dentate line
- Grade II: prolapse out of the anal canal with straining/defaecation but reduce spontaneously
- Grade III: prolapse with straining/defaecation and must be reduced manually
- Grade IV: haemorrhoids which prolapse out of the anal canal and can't be reduced. This is a surgical emergency as grade IV haemorrhoids may strangulate.
Warning
May contain graphic images of human anatomy, medical conditions and medical procedures. Viewing discretion is advised.
Haemorrhoids
Management
- Increasing dietary fibre is important.
- Some patients may find topical steroids (such as Proctosedyl®), sitz baths or simple analgesia useful.
- If persistent or severe, refer to a colorectal or general surgeon for rubber band ligation, sclerotherapy, cauterisation or excisional haemorrhoidectomy.